Abstract
Obsessive–compulsive disorder (OCD) is a neuropsychiatric disorder characterized b–y recurrent and distinctive obsessions and/or compulsions. The etiologies remain unclear. Recent findings have shown that oxidative stress, inflammation, and the glutamatergic pathway play key roles in the causes of OCD. However, first-line therapies include cognitive–behavioral therapy but only 40% of the patients respond to this first-line therapy. Research for a new treatment is mandatory. This review focuses on the potential effects of lithium, as a potential therapeutic strategy, on OCD and some of the presumed mechanisms by which lithium provides its benefit properties. Lithium medication downregulates GSK-3β, the main inhibitor of the WNT/β-catenin pathway. The activation of the WNT/β-catenin could be associated with the control of oxidative stress, inflammation, and glutamatergic pathway. Future prospective clinical trials could focus on lithium and its different and multiple interactions in OCD.
Similar content being viewed by others
Introduction
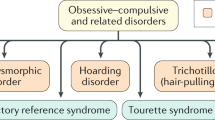
Obsessive–compulsive disorder (OCD) is a neuropsychiatric disorder that affects around 1–2% of the population in their lifetime1. OCD is characterized by recurrent and distinctive obsessions and/or compulsions and causes significant problems for patients and their families. OCD is one of the most common mental health disorders in the world2. OCD reduces the quality of life, increases the recourse of care services, and impairs social functioning. The presence of mood disorders, depression, anxiety, impulse control disorders, sleep disturbance, and personality disorders could be associated with OCD and exhibit comorbid conditions3. These comorbidities can be correlated with social difficulties and can have a major impact on health-related quality of life4. The risk of suicide is increased in OCD5. Efficacious treatments are needed to face the debilitating nature of OCD6. The etiologies of OCD remain unclear, but there are several functional disorders in many structures such as the brain’s orbitofrontal cortex, limbic system, basal ganglia and thalamus, and neurotransmitters7.
Nevertheless, the links between neuro-anatomical and biochemical models have not yet been well-established definitively8.
In recent years, oxidative stress and free radicals9, inflammation10, and the glutamatergic pathway11 have been shown to play key roles in the causes of OCD.
First-line therapies include cognitive-behavioral therapy12. Augmentation strategies with antipsychotics could provide some benefits in at least a third of patients in the case of treatment resistance. Only 40–60% of the patients respond to first-line therapy and research for new treatment beyond current guidelines is mandatory13.
This review focuses on the potential effects of lithium, as a potential therapeutic strategy, on OCD and some of the presumed mechanisms by which lithium provides its beneficial properties.
Lithium, which was introduced in 1949, is the main commonly used drug for the treatment of chronic mental illnesses, such as bipolar disorder, characterized by depressive and manic cycles. Lithium remains the first-line therapy for manic-depressive illness, bipolar disorder14, traumatic brain injury15, and numerous neurodegenerative diseases, such as Alzheimer’s, Huntington’s, and Parkinson’s diseases16. In the acute treatment of mania, the efficacy of lithium is well established17. Several studies have shown that prophylactically lithium can reduce manic relapses, even if its efficacy is significantly lower in the reduction of depressive relapses18. Moreover, other studies have presented that therapy by lithium could reduce suicides and suicide attempts in patients with mood disorders19. Lithium therapeutic mechanisms remain complex, including several pathways and gene expression, such as neurotransmitters and receptors, circadian modulation, ion transport, and signal transduction processes20.
Thus, recent advances seem to show that the benefits of lithium extend beyond just the treatment of mood. Neuroprotection against excitotoxicity or brain damage is another role of lithium21. However, in contrast, several reports have presented that a high dose of lithium could induce irreversible neurotoxicity effects22. Excessive intake or impaired excretion could result in lithium accumulation. Lithium is mainly susceptible to accumulation in bone, muscle, liver, thyroid, and kidney23. Dehydration, febrile illness, or gastrointestinal loss can lead to elevated lithium levels in serum24. Renal toxicity is more common in patients on chronic lithium therapy with nephrogenic diabetes insipidus25. The neurologic effects are hyperreflexia, nystagmus, or ataxia and remain mostly reversible24. Other troubles are reversible cardiovascular effects (QT prolongation, intraventricular conduction defects)26, gastrointestinal effects27, and endocrine effects28. But, low doses of lithium are correlated with lower side-effects29.
Pathophysiology of OCD
OCD and oxidative stress
The oxidative stress process presents an imbalance between production and elimination of reactive metabolites and free radicals (ROS and RNS)30. ROS production is due to cell damages by nitration and oxidation of several lipids, proteins, and DNA. The NADPH oxidase (NOX) enzyme involves ROS by the oxidation of intracellular NDAPH to NADP + . Intracellular and extracellular environmental conditions are modulated by ROS production31. Mitochondrial dysfunction associated with excessive ROS production and a diminution in ATP production characterize the oxidative stress process32. Inflammation markers, such as leukocytes, are recruited from the damage sites and then participate in the increased uptake of oxygen for the release of ROS and thus its accumulation. NOX, activated by the inflammation process, enhances oxidative stress32,33.
The main antioxidants are superoxide dismutase (SOD), glutathione peroxides, and catalase. SOD is synthesized in response to oxidative stress and acts as an antioxidant, but its elevation in intracellular conditions increases cell damage by a generation of H2O234. Glutathione is one of the first-line defense against oxidative stress. Glutathione peroxidases are selenoenzymes that catalyze the reduction in hydroperoxide at the expense of gluthatione34. The heme-containing enzyme catalase has a major role in the removal of hydrogen peroxide35. They protect bio-membranes against oxidative attack, lipid peroxidation by H2O2, and slows down H2O2-dependent free-radical attack on lipids36.
Free radicals (ROS and RNS) induce a decrease in synaptic efficacy37 by affecting excitatory and inhibitory synaptic potentials38. Free radicals deteriorate membrane lipids by lipid peroxidation, cause ATP depletion, DNA damage and neuronal dysregulation39. The brain and nervous system are especially prone to free-radical-induced damage, due to their highly oxygenated organ function40 and low catalase activities41. The brain presents a large amount of iron and polyunsaturated fatty acids and a moderate amount of SOD and glutathione peroxides34. Several studies have shown that free-radical-mediated neuronal dysregulation plays a key role in the pathophysiology of psychiatric diseases by increased SOD activity levels, such as in schizophrenia42. The comorbidity observed in OCD raises this possibility of basal ganglia involvement43. Major depression presents increased monoamine oxidase activity and elevated antioxidant levels44. Recent studies have shown that SOD levels were significantly higher in OCD patients compared to the control group34. A higher production of reactive oxygen metabolites, such as the superoxide anion, affects catalase activity45, and an increase in production of hydroxyl ions reduces catalase activity46. Numerous studies have shown a link between OCD and oxidative stress by the involvement of free radicals and antioxidant defense34,44. Moreover, free radicals damage the cell structure and extracellular matrix compounds by disrupting the genetic structure, oxidative stress, mitochondrial dysfunction, and impaired metabolism9.
OCD and inflammation
Numerous evidence has shown an important role played by the immune system (i.e. inflammation) in the etiology of psychiatric disorders47. The link between the immune system and inflammation in OCD pathophysiology is recent and had emerged in the early nineties11. Indeed, the pediatric autoimmune neuropsychiatric disorder associated with group A β-hemolytic streptococcus (GABHS) (PANDAS) and thus the recalled pediatric acute neuropsychiatric syndrome (PANS) have highlighted that several agents rather than streptococcus could be involved in these acute-onset forms of OCD48. The hypothesis for PANS and PANDAS was a link between gangliosides in basal ganglia neurons and the GABHS and/or other agent48. Other studies have presented evidence of inflammatory and immune system increase in pediatric OCD by higher monocytes and CD16 + monocytes compared to healthy control subjects49.
Nevertheless, the relevance of neuro-inflammation and autoimmunity in OCD seems not limited to subsets of pediatric and acute onset forms of OCD but could be of interest in adults50. The role of inflammation in OCD has been strengthened by the higher rate of anti-basal ganglia antibodies (ABGA) in patients with primary OCD versus control subjects51. Moreover, significantly increased levels of cytokines and inflammatory agents have been observed in OCD patients, such as IL-2/4/6/10 and TNF-α, compared to controls52. In a recent study using positron emission tomography (PET) imagery, the presence of inflammation in the cortico-striatal-thalamo-cortical circuit was shown to induce microglial cell activation in OCD patients10.
OCD and microglial dysregulation
Microglia are the brain’s resident immune cells. They are small cells of macrophage lineage originating from hematopoietic progenitors present in the brain. They can be identified in brain tissue by their expression of numerous macrophage markers53. Microglia have been presumed to be quiescent under physiological conditions and activated upon immune stimulation. They act in the regulation of neurogenesis54, neuronal function, and homeostasis under physiological conditions and in the absence of inflammation55. The dysregulated activation of microglia leads to infiltration of the brain by macrophages under pathological conditions55. A specific role for microglia in OCD has been suggested in mouse models56. However, this mechanism remains unclear.
OCD and the glutamatergic pathway
Glutamatergic dysfunction is becoming the principal focus o pharmacological research in the OCD field. Glutamate is an amino acid responsible for the brain’s primary excitatory neurotransmission and is considered as the main neurotransmitter within the cortico-striatal-thalamic circuit involved in OCD57. Glutamatergic neurons are embedded in every brain circuit in comparison to dopamine and serotonin, which are used by a small minority of neural cells in the brain. Numerous evidence has shown a glutamatergic dysfunction in OCD11,58.
Glutamate is the main excitatory neurotransmitter in the brain and is present in more than 50% of synapses. This signaling plays a major role in neuronal plasticity, memory, and learning59. Rapid neurotoxicity enhanced by neuronal excitotoxin has been observed with abnormal glutamate levels60.
In neurons, glutamate is stored in synaptic vesicles from which it is released. The release of glutamate leads to increased glutamate concentration in the synaptic cleft to bind ionotropic glutamate receptors. The main consistent candidate gene in OCD is the SLC1A1 (solute carrier, family 1, member 1) gene61. SLC1A1 encodes for the neuronal excitatory Na + -dependent amino acid transporter 3 (EAAT3). EAAT1 and EAAT2 are the main astrocyte glutamate transporters, whereas EAAT3 is the major neuronal glutamate transporter. Glutamate is converted into glutamine in astrocytes and thus releases it. Then, glutamine is taken up by neurons to be re-converted into glutamate62. The role of the EAAT3 is to control glutamate spillover, which affects pre-synaptic N-methyl-D-aspartate (NMDA) and metabotropic glutamate receptors activity63,64. EAAT3 activity is dysregulated by the overexpression of GSK-3β65.
Increased levels of glutamate in adult unmedicated patients with OCD have been shown in cerebrospinal fluid (CSF)66,67. Moreover, studies based on magnetic resonance spectroscopy (MRS) have observed increased glutamate and related components in brain areas, including central nodes of the cortico-striatal-thalamo-cortical circuit in OCD patients11,68. In addition, genetic studies have also involved a correlation of glutamatergic genes with OCD69.
Activation of the canonical WNT pathway by lithium: a potential therapeutic strategy
Lithium and GSK-3β
A recent study has observed that mutant murine models of OCD presented increased GSK-3β activity and thus its inhibition could be a treatment of perseverative behaviors70.
Glycogen synthase kinase-3β (GSK-3β) is a serine/threonine kinase that is involved in numerous intracellular signaling pathways. Dysfunction of GSK-3β is involved in the pathogenesis of several diseases, including neuropsychiatric disorders71. GSK-3β is a regulator of several pathways such as inflammation, neuronal polarity, or either cell membrane signaling72. GSK3β is known to be the major inhibitor of the canonical WNT/β-catenin pathway73. The name WNT is derived from Wingless drosophila melanogaster and its mouse homolog Int. The WNT pathway is involved in numerous signaling and regulating pathways, such as embryogenesis, cell proliferation, migration and polarity, apoptosis, and organogenesis74. However, during numerous pathological states, the WNT pathway can be dysregulated, such as in inflammatory, metabolic and neurological disorders, tissue fibrosis, and cancers75. GSK-3β downregulates the canonical WNT/β-catenin pathway by inhibiting β-catenin cytosolic stabilization and its translocation in the nucleus76. Moreover, several studies have shown a link between neuroinflammation and the augmentation of the GSK-3β activity and in parallel the decrease of the WNT/β-catenin pathway and the protein kinase B (Akt) pathway (Fig. 1)77.
Lithium at concentrations of 1–2 mM can inhibit GSK-3β activity78,79,80. Lithium reduces GSK-3β activity by increasing the inhibitory phosphorylation of GSK3β and through direct activation of the Akt pathway. The activation of Akt modulates forkhead bow class O (FOXO)and Bcl-2 associated death protein (Bad) (a pro-apoptotic protein of the Bcl-2 family)81,82.
Lithium and the WNT/β-catenin pathway
Therapeutic concentrations of the GSK-3β inhibitor lithium lead to the increase in β-catenin levels83,84 and then promotes β-catenin transcriptional activity16,85. In the brain of a mouse, the over-expression of β-catenin levels mimics the anti-depressant-like effects of lithium86, while the knockout of β-catenin leads to a depression-like phenotype87,88.
Lithium in OCD
Lithium and oxidative stress
The energy and glucose metabolisms involved during oxidative stress are mainly regulated by the intracellular FOXO transcription factors (FOXO1, 3a, 4)89. The interaction between β-catenin and FOXO transcription factors promotes cell quiescence and cell cycle arrest. Β-catenin blocks its transcriptional complex with TCF/LEF through the interaction with FOXO-induced ROS90. Β-cateni does not translocate to the nucleus and thus accumulates in the cytosol, leading to the inactivation of the WNT/β-catenin pathway91,92. A previous study has found that lithium can reduce FOXO3a transcriptional activity and can decrease the level of active FOXO3a93. Thus, by inactivating GSK3-β, activating the WNT/β-catenin pathway, and reducing the FOXO, lithium could participate in the reduction of oxidative stress in OCD.
Furthermore, several in vitro studies have shown that lithium administration could inhibit hydrogen peroxide-induced cell death as well as obstruct lipid peroxidation and protein oxidation in cortical cells94,95,96,97,98,99. Moreover, lithium can act as an anti-oxidant by increasing the CHS levels in neurons of rat dopaminergic N2795,99.
Lithium and inflammation
Through the inhibition of GSK-3β and thus the upregulation of the WNT/β-catenin pathway, the lithium administration could involve a diminution of the neuro-inflammation by acting on the NF-ϰB pathway. The activation of the WNT pathway cascade restrains inflammation and leads to neuroprotection via interactions between microglia/macrophages and astrocytes (Fig. 2)100,101.
Several studies have shown negative crosstalk between the WNT/β-catenin pathway and the NF-ϰB signaling pathway102. The NF-ϰB transcription factor family consists of five members in the cytosol under non-activated conditions: NF-ϰB1 (p50/p105), NF-ϰB 2 (p52/p100), RelA (p65), RelB, and c-Rel103. Β-CATENIN can form a complex with RelA and p50 to decrease the activity of the NF-ϰB signaling104. Moreover, by interacting with the PI3K, β-catenin inhibits the functional activity of NF-ϰB105. This inhibitory function of β-catenin on NF-ϰB activity has been observed in numerous cell types, such as fibroblasts, epithelial cells, hepatocytes, and osteoblasts102. In parallel, the overactivation of GSK-3β leads to an inhibition of the β-catenin and then activation of the NF-ϰB pathway106. The potential protective action of β-catenin was due to the activation of the PI3K/Akt pathway and thus the reduction of TLR4-driven inflammatory response in hepatocytes107. NF-ϰB activation leads to the inhibition of the complex β-catenin/TCF/LEF by the upregulation of LZTS2 in cancer cells108. DKK, a WNT inhibitor, was a target gene of the NF-ϰB pathway leading to a negative feedback to diminish the β-catenin signaling109.
A recent study has presented that the WNT pathway appeared to be one of the main mechanisms of the action of lithium in adipose cells, and this interaction is done by the inhibition of PPARγ expression110. PPARs are ligand-activated transcription factors that bind PPRE (PPAR-response elements). PPARs are involved in numerous pathophysiological processes, such as cell differentiation, protein metabolism, lipids metabolism, carcinogenesis111,112, adipocyte differentiation, insulin sensitivity, and inflammation113,114. PPARγ ligands, such as thiazolidinediones (TZDs), are able to decrease inflammatory activity115.
A negative crosstalk has been well described between PPARγ and the WNT pathway32,73,116,117. The PI3K/Akt pathway, which is positively induced by β-catenin118,119, acts by phosphorylating GSK-3β to negatively regulate PPARγ expression120. PPARγ agonists decrease β-catenin expression by overactivating GSK-3β121. Moreover, PPARγ agonists activate Dickkopf-1 (DKK1) activity to decrease the canonical WNT/β-catenin pathway and then inhibit fibroblast differentiation122. Furthermore, PPARγ agonists activate GSK-3β to decrease β-catenin expression121.
Lithium and the glutamatergic pathway
Lithium administration has been also associated with an influence on the levels of proapoptotic proteins. Bax, named Bcl-2 associated C protein, is a key modulator promoting apoptosis by binding to and antagonizing the Bcl-2 protein. The tumor suppressor protein, p53, targets Bcl-2 and Bax and then promotes growth arrests and cell death in response to cell damage (Fig. 2)123.
Several studies have demonstrated that the neuroprotective effects of lithium could be attributed to increased Bcl-2 levels. Indeed, lithium therapy of cultured cerebellar granule cells increased mRNA and protein levels of Bcl-2, and the Bcl-2/Bax protein level ratio increased by 5-fold after treatment duration for 5–7 days124. The increase in Bcl-2 expression leads to neurogenesis in the hippocampus and entorhinal cortex in mice by the increase of axon diameters and neurite growth on the CA3 area of the hippocampus and increased myelination in the entorhinal cortex125. Lithium can also act by stimulating anti-apoptotic-increasing Bcl-2 levels and reducing Bax126. The phosphorylation of Bcl 2 at serine 70 is needed for a complete anti-apoptotic function127 and lithium has this ability128. Lithium inhibits Bcl-2 dephosphorylation and caspase-2 activation through the reduction of the protein phosphatase-2A activity128.
Glutamate excitotoxicity has been associated with the upregulation of Bax and p53 and the downregulation of Bcl-2124. The apoptosis attributed to glutamate was preceded by the increase in activator protein-1 (AP-1) caused by the activation of c-Jun N-terminal kinase (JNK) and p38 mitogen-activated protein kinase (MAP kinase) and phosphorylation of c-Jun and p53129.
By inhibiting GSK-3β activity, lithium acts as a powerful regulator of EAAT3 and thus of the regulation of NMDA receptors130. Moreover, a direct potential way could be the inhibition of presynaptic NMDA receptors and thus the activation of postsynaptic AMPA receptors by the release of glutamate. This mechanism is followed by the activation of the influx of calcium and secretion of brain-derived neurotrophic factor (BDNF). Lithium stimulated the release of the excitatory neurotransmitter, glutamate, from cerebral cortex slices131. This release was accompanied by an increase in inositol 1,4,5-trisphosphate [Ins(1,4,5)P3] accumulation. The increase in Ins(1,4,5)P3 accumulation was caused by the selective activation of the N-methyl-D-aspartate (NMDA) receptor/channel by glutamate. Activation of the NMDA receptor is known to cause increased Ins(1,4,5)P3 accumulation132. Thus, BDNF stimulates the receptor tyrosine kinase B (TrkB), leading to neuronal survival and differentiation133.
Activated BDNF-TrkB signaling leads to stimulation of the Akt/mTOR pathway, causing activation of the WNT/β-catenin pathway and enhancing synaptic proteins134. The few therapeutic levels of lithium activate the BDNF-TrkB signaling and then the Akt/mTOR signaling to protect neurons from glutamate excitotoxicity135. Lithium inhibits excessive glutamate, NMDA receptor-mediated calcium influx in neurons and reduces NR2B subunit tyrosine phosphorylation by the Src/Fyn kinase136.
PPARγ antagonists can block the increase of PPARγ DNA binding activity and antioxidant enzymatic activities (SOD), inhibiting the protection of PPARγ activation in OGD-exposed neurons137. Other mechanisms by which these PPARγ agonists prevent oxidative stress include a decrease in iNOS activity, NFκB blockade, inhibition of TNF-α release, or activation of nuclear factor (erythroid-derived 2)-like 2 (Nrf2)138. By the negative crosstalk between WNT and PPARγ, lithium administration, by inhibiting the GSK-3β could act as a PPARγ antagonist and lead to an increase in the WNT pathway, resulting in diminution of oxidative stress.
Conclusion
Currently, few studies have studied lithium as a possible alternative therapeutic way to treat OCD patients. However, in low doses, lithium may appear to be interesting against OCD because of its potential inhibitory effect on oxidative stress, inflammation, and the glutamatergic pathway.
No study has still reported the expression of the WNT/β pathway in OCD. Nevertheless, the overactivity of the GSK-3β, the main inhibitor of the WNT pathway, in OCD patients is consistent with a downregulation of the WNT pathway in this disease. By stimulating the WNT/β pathway, through the inhibition of GSK-3β, lithium could be an innovative therapeutic way in OCD. Future prospective studies could focus on lithium and its different and multiple interactions in OCD.
References
Ruscio, A. M., Stein, D. J., Chiu, W. T. & Kessler, R. C. The epidemiology of obsessive-compulsive disorder in the National Comorbidity Survey Replication. Mol. Psychiatry 15, 53–63 (2010).
De Putter, L. M. S. & Koster, E. H. W. The effects of obsessive-compulsive symptoms and disorder-relevant stimuli on the dynamics of selective attention. J. Obsessive-Compuls. Relat. Disord. 15, 74–84 (2017).
Termine, C., Selvini, C., Rossi, G. & Balottin, U. Emerging treatment strategies in tourette syndrome: what’s in the pipeline? Int. Rev. Neurobiol. 112, 445–480 (2013).
Müller-Vahl, K. et al. Health-related quality of life in patients with gilles de la Tourette’s syndrome. Mov. Disord. J. Mov. Disord. Soc. 25, 309–314 (2010).
Fernández de la Cruz, L. et al. Suicide in obsessive-compulsive disorder: a population-based study of 36 788 Swedish patients. Mol. Psychiatry 22, 1626–1632 (2017).
McHugh, R. K., Whitton, S. W., Peckham, A. D., Welge, J. A. & Otto, M. W. Patient preference for psychological vs pharmacologic treatment of psychiatric disorders: a meta-analytic review. J. Clin. Psychiatry 74, 595–602 (2013).
Bokor, G. & Anderson, P. D. Obsessive-compulsive disorder. J. Pharm. Pract. 27, 116–130 (2014).
Bloch, M. H. et al. Meta-analysis: hoarding symptoms associated with poor treatment outcome in obsessive-compulsive disorder. Mol. Psychiatry 19, 1025–1030 (2014).
Alici, D. et al. Evaluation of oxidative metabolism and oxidative DNA damage in patients with obsessive-compulsive disorder. Psychiatry Clin. Neurosci. 70, 109–115 (2016).
Attwells, S. et al. Inflammation in the neurocircuitry of obsessive-compulsive disorder. JAMA Psychiatry 74, 833–840 (2017).
Grassi, G. & Pallanti, S. Current and up-and-coming pharmacotherapy for obsessive-compulsive disorder in adults. Expert Opin. Pharmacother. 19, 1541–1550 (2018).
Fineberg, N. A. et al. Obsessive-compulsive disorder (OCD): practical strategies for pharmacological and somatic treatment in adults. Psychiatry Res. 227, 114–125 (2015).
Pallanti, S., Grassi, G. & Cantisani, A. Emerging drugs to treat obsessive-compulsive disorder. Expert Opin. Emerg. Drugs 19, 67–77 (2014).
Lähteenvuo, M. et al. Real-world effectiveness of pharmacologic treatments for the prevention of rehospitalization in a Finnish nationwide cohort of patients with bipolar disorder. JAMA Psychiatry 75, 347–355 (2018).
Leeds, P. R. et al. A new avenue for lithium: intervention in traumatic brain injury. ACS Chem. Neurosci. 5, 422–433 (2014).
Marmol, F. Lithium: bipolar disorder and neurodegenerative diseases possible cellular mechanisms of the therapeutic effects of lithium. Prog. Neuropsychopharmacol. Biol. Psychiatry 32, 1761–1771 (2008).
Young, A. H. & Hammond, J. M. Lithium in mood disorders: increasing evidence base, declining use? Br. J. Psychiatry J. Ment. Sci. 191, 474–476 (2007).
Smith, L. A., Cornelius, V., Warnock, A., Bell, A. & Young, A. H. Effectiveness of mood stabilizers and antipsychotics in the maintenance phase of bipolar disorder: a systematic review of randomized controlled trials. Bipolar Disord. 9, 394–412 (2007).
Baldessarini, R. J. et al. Decreased risk of suicides and attempts during long-term lithium treatment: a meta-analytic review. Bipolar Disord. 8, 625–639 (2006).
Pisanu, C., Melis, C. & Squassina, A. Lithium pharmacogenetics: where do we stand? Drug Dev. Res. 77, 368–373 (2016).
Zhu, Z.-F., Wang, Q.-G., Han, B.-J. & William, C. P. Neuroprotective effect and cognitive outcome of chronic lithium on traumatic brain injury in mice. Brain Res. Bull. 83, 272–277 (2010).
Donaldson, I. M. & Cuningham, J. Persisting neurologic sequelae of lithium carbonate therapy. Arch. Neurol. 40, 747–751 (1983).
Horton, S., Tuerk, A., Cook, D., Cook, J. & Dhurjati, P. Maximum recommended dosage of lithium for pregnant women based on a PBPK model for lithium absorption. Adv. Bioinforma. 2012, 352729 (2012).
Ott, M., Stegmayr, B., Salander Renberg, E. & Werneke, U. Lithium intoxication: incidence, clinical course and renal function - a population-based retrospective cohort study. J. Psychopharmacol. Oxf. Engl. 30, 1008–1019 (2016).
Erden, A. et al. Lithium intoxication and nephrogenic diabetes insipidus: a case report and review of literature. Int. J. Gen. Med. 6, 535–539 (2013).
Canan, F. et al. Lithium intoxication related multiple temporary ecg changes: A case report. Cases J. 1, 156 (2008).
Mohandas, E. & Rajmohan, V. Lithium use in special populations. Indian J. Psychiatry 49, 211–218 (2007).
Kibirige, D., Luzinda, K. & Ssekitoleko, R. Spectrum of lithium induced thyroid abnormalities: a current perspective. Thyroid Res. 6, 3 (2013).
Abou-Saleh, M. T. & Coppen, A. The efficacy of low-dose lithium: clinical, psychological and biological correlates. J. Psychiatr. Res. 23, 157–162 (1989).
Duracková, Z. Some current insights into oxidative stress. Physiol. Res. 59, 459–469 (2010).
Jabs, T. Reactive oxygen intermediates as mediators of programmed cell death in plants and animals. Biochem Pharm. 57, 231–245 (1999).
Vallée, A. & Lecarpentier, Y. Crosstalk between peroxisome proliferator-activated receptor gamma and the canonical WNT/β-catenin pathway in chronic inflammation and oxidative stress during carcinogenesis. Front Immunol. 9, 745 (2018).
Weyemi, U. et al. ROS-generating NADPH oxidase NOX4 is a critical mediator in oncogenic H-Ras-induced DNA damage and subsequent senescence. Oncogene 31, 1117–1129 (2012).
Behl, A., Swami, G., Sircar, S. S., Bhatia, M. S. & Banerjee, B. D. Relationship of possible stress-related biochemical markers to oxidative/antioxidative status in obsessive-compulsive disorder. Neuropsychobiology 61, 210–214 (2010).
Simon, R. H., Scoggin, C. H. & Patterson, D. Hydrogen peroxide causes the fatal injury to human fibroblasts exposed to oxygen radicals. J. Biol. Chem. 256, 7181–7186 (1981).
Ursini, F. et al. Diversity of glutathione peroxidases. Methods Enzymol. 252, 38–53 (1995).
Rana, S. V. S., Allen, T. & Singh, R. Inevitable glutathione, then and now. Indian J. Exp. Biol. 40, 706–716 (2002).
Pellmar, T. C. Peroxide alters neuronal excitability in the CA1 region of guinea-pig hippocampus in vitro. Neuroscience 23, 447–456 (1987).
Halliwell, B. Oxidants and human disease: some new concepts. FASEB J. Publ. Fed. Am. Soc. Exp. Biol. 1, 358–364 (1987).
Pellmar, T. C., Neel, K. L. & Lee, K. H. Free radicals mediate peroxidative damage in guinea pig hippocampus in vitro. J. Neurosci. Res. 24, 437–444 (1989).
Paul, L. A., Fulton, A. M. & Heppner, G. H. Reactive oxygen-mediated damage to murine mammary tumor cells. Mutat. Res. 215, 223–234 (1989).
Graham, D. G. Oxidative pathways for catecholamines in the genesis of neuromelanin and cytotoxic quinones. Mol. Pharm. 14, 633–643 (1978).
Yao, J. K., Reddy, R. & van Kammen, D. P. Reduced level of plasma antioxidant uric acid in schizophrenia. Psychiatry Res. 80, 29–39 (1998).
Kuloglu, M. et al. Antioxidant enzyme activities and malondialdehyde levels in patients with obsessive-compulsive disorder. Neuropsychobiology 46, 27–32 (2002).
Beech H., Vaughan C. The behavioral treatment of obsessional states. Wiley: london, 1970.
Pigeolet, E. et al. Glutathione peroxidase, superoxide dismutase, and catalase inactivation by peroxides and oxygen derived free radicals. Mech. Ageing Dev. 51, 283–297 (1990).
Khandaker, G. M., Dantzer, R. & Jones, P. B. Immunopsychiatry: important facts. Psychol. Med. 47, 2229–2237 (2017).
Chiarello, F., Spitoni, S., Hollander, E., Matucci Cerinic, M. & Pallanti, S. An expert opinion on PANDAS/PANS: highlights and controversies. Int. J. Psychiatry Clin. Pr. 21, 91–98 (2017).
Rodríguez, N. et al. Inflammatory dysregulation of monocytes in pediatric patients with obsessive-compulsive disorder. J. Neuroinflammation 14, 261 (2017).
Mataix-Cols, D. et al. A total-population multigenerational family clustering study of autoimmune diseases in obsessive-compulsive disorder and tourette’s/chronic tic disorders. Mol. Psychiatry 23, 1652–1658 (2018).
Pearlman, D. M., Vora, H. S., Marquis, B. G., Najjar, S. & Dudley, L. A. Anti-basal ganglia antibodies in primary obsessive-compulsive disorder: systematic review and meta-analysis. Br. J. Psychiatry J. Ment. Sci. 205, 8–16 (2014).
Rao, N. P. et al. Plasma cytokine abnormalities in drug-naïve, comorbidity-free obsessive-compulsive disorder. Psychiatry Res. 229, 949–952 (2015).
Wolf, S. A., Boddeke, H. W. G. M. & Kettenmann, H. Microglia in physiology and disease. Annu Rev. Physiol. 79, 619–643 (2017).
Sierra, A. et al. Microglia shape adult hippocampal neurogenesis through apoptosis-coupled phagocytosis. Cell Stem Cell. 7, 483–495 (2010).
Frick, L. R., Williams, K. & Pittenger, C. Microglial dysregulation in psychiatric disease. Clin. Dev. Immunol. 2013, 608654 (2013).
Greer, J. M. & Capecchi, M. R. Hoxb8 is required for normal grooming behavior in mice. Neuron 33, 23–34 (2002).
Ting, J. T. & Feng, G. Neurobiology of obsessive-compulsive disorder: insights into neural circuitry dysfunction through mouse genetics. Curr. Opin. Neurobiol. 21, 842–848 (2011).
Marinova, Z., Chuang, D.-M. & Fineberg, N. Glutamate-modulating drugs as a potential therapeutic strategy in obsessive-compulsive disorder. Curr. Neuropharmacol. 15, 977–995 (2017).
Javitt, D. C. et al. Translating glutamate: from pathophysiology to treatment. Sci. Transl. Med 3, 102mr2 (2011).
Sanacora, G., Zarate, C. A., Krystal, J. H. & Manji, H. K. Targeting the glutamatergic system to develop novel, improved therapeutics for mood disorders. Nat. Rev. Drug Disco. 7, 426–437 (2008).
Arnold, P. D., Sicard, T., Burroughs, E., Richter, M. A. & Kennedy, J. L. Glutamate transporter gene SLC1A1 associated with obsessive-compulsive disorder. Arch. Gen. Psychiatry 63, 769–776 (2006).
Daikhin, Y. & Yudkoff, M. Compartmentation of brain glutamate metabolism in neurons and glia. J. Nutr. 130, 1026S–1031SS (2000).
Scimemi, A., Tian, H. & Diamond, J. S. Neuronal transporters regulate glutamate clearance, NMDA receptor activation, and synaptic plasticity in the hippocampus. J. Neurosci. J. Soc. Neurosci. 29, 14581–14595 (2009).
Wu, K., Hanna, G. L., Rosenberg, D. R. & Arnold, P. D. The role of glutamate signaling in the pathogenesis and treatment of obsessive-compulsive disorder. Pharm. Biochem Behav. 100, 726–735 (2012).
Kim, M.-S. et al. Nerve growth factor (NGF) regulates activity of nuclear factor of activated T-cells (NFAT) in neurons via the phosphatidylinositol 3-kinase (PI3K)-Akt-glycogen synthase kinase 3β (GSK3β) pathway. J. Biol. Chem. 289, 31349–31360 (2014).
Ting, J. T. & Feng, G. Glutamatergic synaptic dysfunction and obsessive-compulsive disorder. Curr. Chem. Genomics. 2, 62–75 (2008).
Chakrabarty, K., Bhattacharyya, S., Christopher, R. & Khanna, S. Glutamatergic dysfunction in OCD. Neuropsychopharmacol. Publ. Am. Coll. Neuropsychopharmacol. 30, 1735–1740 (2005).
Starck, G. et al. A 1H magnetic resonance spectroscopy study in adults with obsessive compulsive disorder: relationship between metabolite concentrations and symptom severity. J. Neural Transm. Vienna Austria 1996 115, 1051–1062 (2008).
Pauls, D. L., Abramovitch, A., Rauch, S. L. & Geller, D. A. Obsessive-compulsive disorder: an integrative genetic and neurobiological perspective. Nat. Rev. Neurosci. 15, 410–424 (2014).
Thompson, S. L. & Dulawa, S. C. Dissecting the roles of β-arrestin2 and GSK-3 signaling in 5-HT1BR-mediated perseverative behavior and prepulse inhibition deficits in mice. Plos ONE. 14, e0211239 (2019).
Giese, K. P. GSK-3: a key player in neurodegeneration and memory. IUBMB Life. 61, 516–521 (2009).
Hur, E.-M. & Zhou, F.-Q. GSK3 signalling in neural development. Nat. Rev. Neurosci. 11, 539–551 (2010).
Vallée A., Vallée J.-N., Lecarpentier Y. PPARγ agonists: potential treatment for autism spectrum disorder by inhibiting the canonical WNT/β-catenin pathway. Mol. Psychiatry 2018. https://doi.org/10.1038/s41380-018-0131-4.
Loh, K. M., van Amerongen, R. & Nusse, R. Generating cellular diversity and spatial form: Wnt signaling and the evolution of multicellular animals. Dev. Cell .38, 643–655 (2016).
Oren, O. & Smith, B. D. Eliminating cancer stem cells by targeting embryonic signaling pathways. Stem Cell Rev. 13, 17–23 (2017).
Libro, R., Bramanti, P. & Mazzon, E. The role of the Wnt canonical signaling in neurodegenerative diseases. Life Sci. 158, 78–88 (2016).
Sharma, C., Pradeep, A., Wong, L., Rana, A. & Rana, B. Peroxisome proliferator-activated receptor gamma activation can regulate beta-catenin levels via a proteasome-mediated and adenomatous polyposis coli-independent pathway. J. Biol. Chem. 279, 35583–35594 (2004).
Bauer, M., Alda, M., Priller, J. & Young, L. T., International group for the study of lithium treated patients (IGSLI). Implications of the neuroprotective effects of lithium for the treatment of bipolar and neurodegenerative disorders. Pharmacopsychiatry 36, S250–S254 (2003). Suppl 3.
Rowe, M. K. & Chuang, D.-M. Lithium neuroprotection: molecular mechanisms and clinical implications. Expert Rev. Mol. Med. 6, 1–18 (2004).
Rowe, M. K., Wiest, C. & Chuang, D.-M. GSK-3 is a viable potential target for therapeutic intervention in bipolar disorder. Neurosci. Biobehav Rev. 31, 920–931 (2007).
Alural, B., Ozerdem, A., Allmer, J., Genc, K. & Genc, S. Lithium protects against paraquat neurotoxicity by NRF2 activation and miR-34a inhibition in SH-SY5Y cells. Front Cell Neurosci. 9, 209 (2015).
Beaulieu, J.-M., Gainetdinov, R. R. & Caron, M. G. The Akt-GSK-3 signaling cascade in the actions of dopamine. Trends Pharm. Sci. 28, 166–172 (2007).
Gould, T. D., Chen, G. & Manji, H. K. In vivo evidence in the brain for lithium inhibition of glycogen synthase kinase-3. Neuropsychopharmacol. Publ. Am. Coll. Neuropsychopharmacol. 29, 32–38 (2004).
O’Brien, W. T. et al. Glycogen synthase kinase-3beta haploinsufficiency mimics the behavioral and molecular effects of lithium. J. Neurosci. J. Soc. Neurosci. 24, 6791–6798 (2004).
Jope, R. S. & Johnson, G. V. W. The glamour and gloom of glycogen synthase kinase-3. Trends Biochem Sci. 29, 95–102 (2004).
Gould, T. D. et al. Beta-catenin overexpression in the mouse brain phenocopies lithium-sensitive behaviors. Neuropsychopharmacol. Publ. Am. Coll. Neuropsychopharmacol. 32, 2173–2183 (2007).
Gould, T. D. et al. Generation and behavioral characterization of beta-catenin forebrain-specific conditional knock-out mice. Behav. Brain Res. 189, 117–125 (2008).
Gould, T. D., Quiroz, J. A., Singh, J., Zarate, C. A. & Manji, H. K. Emerging experimental therapeutics for bipolar disorder: insights from the molecular and cellular actions of current mood stabilizers. Mol. Psychiatry 9, 734–755 (2004).
Barthel, A., Schmoll, D. & Unterman, T. G. FoxO proteins in insulin action and metabolism. Trends Endocrinol. Metab. TEM. 16, 183–189 (2005).
Almeida, M., Ambrogini, E., Han, L., Manolagas, S. C. & Jilka, R. L. Increased lipid oxidation causes oxidative stress, increased peroxisome proliferator-activated receptor-gamma expression, and diminished pro-osteogenic Wnt signaling in the skeleton. J. Biol. Chem. 284, 27438–27448 (2009).
Essers, M. A. G. et al. Functional interaction between beta-catenin and FOXO in oxidative stress signaling. Science. 308, 1181–1184 (2005).
Hoogeboom, D. et al. Interaction of FOXO with beta-catenin inhibits beta-catenin/T cell factor activity. J. Biol. Chem. 283, 9224–9230 (2008).
Mao, Z., Liu, L., Zhang, R. & Li, X. Lithium reduces FoxO3a transcriptional activity by decreasing its intracellular content. Biol. Psychiatry 62, 1423–1430 (2007).
Shao, L., Young, L. T. & Wang, J.-F. Chronic treatment with mood stabilizers lithium and valproate prevents excitotoxicity by inhibiting oxidative stress in rat cerebral cortical cells. Biol. Psychiatry 58, 879–884 (2005).
de Vasconcellos, A. P. S. et al. Chronic lithium treatment has antioxidant properties but does not prevent oxidative damage induced by chronic variate stress. Neurochem Res. 31, 1141–1151 (2006).
Cui, J., Shao, L., Young, L. T. & Wang, J.-F. Role of glutathione in neuroprotective effects of mood stabilizing drugs lithium and valproate. Neuroscience 144, 1447–1453 (2007).
Frey, B. N. et al. Increased oxidative stress and DNA damage in bipolar disorder: a twin-case report. Prog. Neuropsychopharmacol. Biol. Psychiatry 31, 283–285 (2007).
Machado-Vieira, R. et al. Oxidative stress parameters in unmedicated and treated bipolar subjects during initial manic episode: a possible role for lithium antioxidant effects. Neurosci. Lett. 421, 33–36 (2007).
Kim, Y.-H., Rane, A., Lussier, S. & Andersen, J. K. Lithium protects against oxidative stress-mediated cell death in α-synuclein-overexpressing in vitro and in vivo models of parkinson’s disease. J. Neurosci. Res. 89, 1666–1675 (2011).
Halleskog, C. et al. WNT signaling in activated microglia is proinflammatory. Glia 59, 119–131 (2011).
L’episcopo, F. et al. A Wnt1 regulated frizzled-1/β-catenin signaling pathway as a candidate regulatory circuit controlling mesencephalic dopaminergic neuron-astrocyte crosstalk: herapeutical relevance for neuron survival and neuroprotection. Mol. Neurodegener. 6, 49 (2011).
Ma, B. & Hottiger, M. O. Crosstalk between Wnt/β-catenin and NF-κB signaling pathway during inflammation. Front Immunol. 7, 378 (2016).
Mitchell, S., Vargas, J. & Hoffmann, A. Signaling via the NFκB system. Wiley Interdiscip. Rev. Syst. Biol. Med. 8, 227–241 (2016).
Deng, J. et al. beta-catenin interacts with and inhibits NF-kappa B in human colon and breast cancer. Cancer Cell. 2, 323–334 (2002).
Liu, J. et al. PI3K is required for the physical interaction and functional inhibition of NF-κB by β-catenin in colorectal cancer cells. Biochem Biophys. Res Commun. 434, 760–766 (2013).
Martin, M., Rehani, K., Jope, R. S. & Michalek, S. M. Toll-like receptor-mediated cytokine production is differentially regulated by glycogen synthase kinase 3. Nat. Immunol. 6, 777–784 (2005).
Manicassamy, S. et al. Activation of beta-catenin in dendritic cells regulates immunity versus tolerance in the intestine. Science. 329, 849–853 (2010).
Cho, H. H. et al. Differential effect of NF-kappaB activity on beta-catenin/Tcf pathway in various cancer cells. FEBS Lett. 582, 616–622 (2008).
Fliniaux, I., Mikkola, M. L., Lefebvre, S. & Thesleff, I. Identification of dkk4 as a target of Eda-A1/Edar pathway reveals an unexpected role of ectodysplasin as inhibitor of Wnt signalling in ectodermal placodes. Dev. Biol. 320, 60–71 (2008).
Rodríguez de la Concepción, M. L., Yubero, P., Iglesias, R., Giralt, M. & Villarroya, F. Lithium inhibits brown adipocyte differentiation. FEBS Lett. 579, 1670–1674 (2005).
Lee, C.-H., Olson, P. & Evans, R. M. Minireview: lipid metabolism, metabolic diseases, and peroxisome proliferator-activated receptors. Endocrinology 144, 2201–2207 (2003).
Marx, N., Duez, H., Fruchart, J.-C. & Staels, B. Peroxisome proliferator-activated receptors and atherogenesis: regulators of gene expression in vascular cells. Circ. Res. 94, 1168–1178 (2004).
Cunard, R. et al. Regulation of cytokine expression by ligands of peroxisome proliferator activated receptors. J. Immunol. Balt. Md. 1950 168, 2795–2802 (2002).
Ricote, M., Li, A. C., Willson, T. M., Kelly, C. J. & Glass, C. K. The peroxisome proliferator-activated receptor-gamma is a negative regulator of macrophage activation. Nature. 391, 79–82 (1998).
Giannini, S., Serio, M. & Galli, A. Pleiotropic effects of thiazolidinediones: taking a look beyond antidiabetic activity. J. Endocrinol. Invest. 27, 982–991 (2004).
Vallée, A., Lecarpentier, Y., Guillevin, R. & Vallée, J.-N. Thermodynamics in gliomas: interactions between the canonical WNT/beta-catenin pathway and PPAR gamma. Front Physiol. 8, 352 (2017).
Vallée A., Lecarpentier Y., Guillevin R., Vallée J.-N. Demyelination in multiple sclerosis: reprogramming energy metabolism and potential PPARγ agonist treatment approaches. Int. J. Mol. Sci. 2018; https://doi.org/10.3390/ijms19041212.
Park, K. S. et al. Neuronal differentiation of embryonic midbrain cells by upregulation of peroxisome proliferator-activated receptor-gamma via the JNK-dependent pathway. Exp. Cell Res. 297, 424–433 (2004).
Vallée, A. & Vallée, J.-N. Warburg effect hypothesis in autism Spectrum disorders. Mol. Brain. 11, 1 (2018).
Grimes, C. A. & Jope, R. S. The multifaceted roles of glycogen synthase kinase 3beta in cellular signaling. Prog. Neurobiol. 65, 391–426 (2001).
Jeon, M., Rahman, N. & Kim, Y.-S. Wnt/β-catenin signaling plays a distinct role in methyl gallate-mediated inhibition of adipogenesis. Biochem Biophys. Res Commun. 479, 22–27 (2016).
Gustafson, B., Eliasson, B. & Smith, U. Thiazolidinediones increase the wingless-type MMTV integration site family (WNT) inhibitor Dickkopf-1 in adipocytes: a link with osteogenesis. Diabetologia 53, 536–540 (2010).
Basu, A. & Haldar, S. The relationship between BcI2, Bax and p53: consequences for cell cycle progression and cell death. Mol. Hum. Reprod. 4, 1099–1109 (1998).
Chen, R. W. & Chuang, D. M. Long term lithium treatment suppresses p53 and Bax expression but increases Bcl-2 expression. A prominent role in neuroprotection against excitotoxicity. J. Biol. Chem. 274, 6039–6042 (1999).
Chen, G., Rajkowska, G., Du, F., Seraji-Bozorgzad, N. & Manji, H. K. Enhancement of hippocampal neurogenesis by lithium. J. Neurochem 75, 1729–1734 (2000).
Youdim, M. B. H. & Arraf, Z. Prevention of MPTP (N-methyl-4-phenyl-1,2,3,6-tetrahydropyridine) dopaminergic neurotoxicity in mice by chronic lithium: involvements of Bcl-2 and Bax. Neuropharmacology 46, 1130–1140 (2004).
Ruvolo, P. P., Deng, X. & May, W. S. Phosphorylation of Bcl2 and regulation of apoptosis. Leukemia 15, 515–522 (2001).
Chen, C.-L., Lin, C.-F., Chiang, C.-W., Jan, M.-S. & Lin, Y.-S. Lithium inhibits ceramide- and etoposide-induced protein phosphatase 2A methylation, Bcl-2 dephosphorylation, caspase-2 activation, and apoptosis. Mol. Pharm. 70, 510–517 (2006).
Chen, R.-W. et al. Regulation of c-Jun N-terminal kinase, p38 kinase and AP-1 DNA binding in cultured brain neurons: roles in glutamate excitotoxicity and lithium neuroprotection. J. Neurochem. 84, 566–575 (2003).
Abousaab, A. & Lang, F. Up-regulation of excitatory amino acid transporters EAAT3 and EAAT4 by lithium sensitive glycogen synthase kinase GSK3ß. Cell Physiol. Biochem Int. J. Exp. Cell Physiol. Biochem Pharm. 40, 1252–1260 (2016).
Dixon, J. F. & Hokin, L. E. Lithium acutely inhibits and chronically up-regulates and stabilizes glutamate uptake by presynaptic nerve endings in mouse cerebral cortex. Proc. Natl Acad. Sci. USA 95, 8363–8368 (1998).
Mayer, M. L. & Miller, R. J. Excitatory amino acid receptors, second messengers and regulation of intracellular Ca2+ in mammalian neurons. Trends Pharm. Sci. 11, 254–260 (1990).
Yoshii, A. & Constantine-Paton, M. Postsynaptic BDNF-TrkB signaling in synapse maturation, plasticity, and disease. Dev. Neurobiol. 70, 304–322 (2010).
Scheuing, L., Chiu, C.-T., Liao, H.-M. & Chuang, D.-M. Antidepressant mechanism of ketamine: perspective from preclinical studies. Front Neurosci. 9, 249 (2015).
Chiu C.-T., et al. The mood stabilizer lithium potentiates the antidepressant-like effects and ameliorates oxidative stress induced by acute ketamine in a mouse model of stress. Int. J. Neuropsychopharmacol 2014; https://doi.org/10.1093/ijnp/pyu102.
Chiu, C.-T. & Chuang, D.-M. Molecular actions and therapeutic potential of lithium in preclinical and clinical studies of CNS disorders. Pharm. Ther. 128, 281–304 (2010).
Zeng, Y. et al. Hyperbaric oxygen preconditioning protects cortical neurons against oxygen-glucose deprivation injury: role of peroxisome proliferator-activated receptor-gamma. Brain Res. 1452, 140–150 (2012).
Heneka, M. T. & Landreth, G. E. PPARs in the brain. Biochim Biophys. Acta. 1771, 1031–1045 (2007).
Author information
Authors and Affiliations
Contributions
All authors listed have contributed to the work and approved it for submission to publication.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationship that could be construed as a potential conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Vallée, A., Vallée, JN. & Lecarpentier, Y. Lithium: a potential therapeutic strategy in obsessive–compulsive disorder by targeting the canonical WNT/β pathway. Transl Psychiatry 11, 204 (2021). https://doi.org/10.1038/s41398-021-01329-3
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41398-021-01329-3
This article is cited by
-
Mitochondrial modulators for obsessive–compulsive and related disorders: a systematic review and meta-analysis
Translational Psychiatry (2022)
-
Lithium bioaccumulation in Lentinus crinitus mycelia grown in media with different lithium sources and pH values
Environmental Science and Pollution Research (2022)